
Written by Dr. Diane Mueller
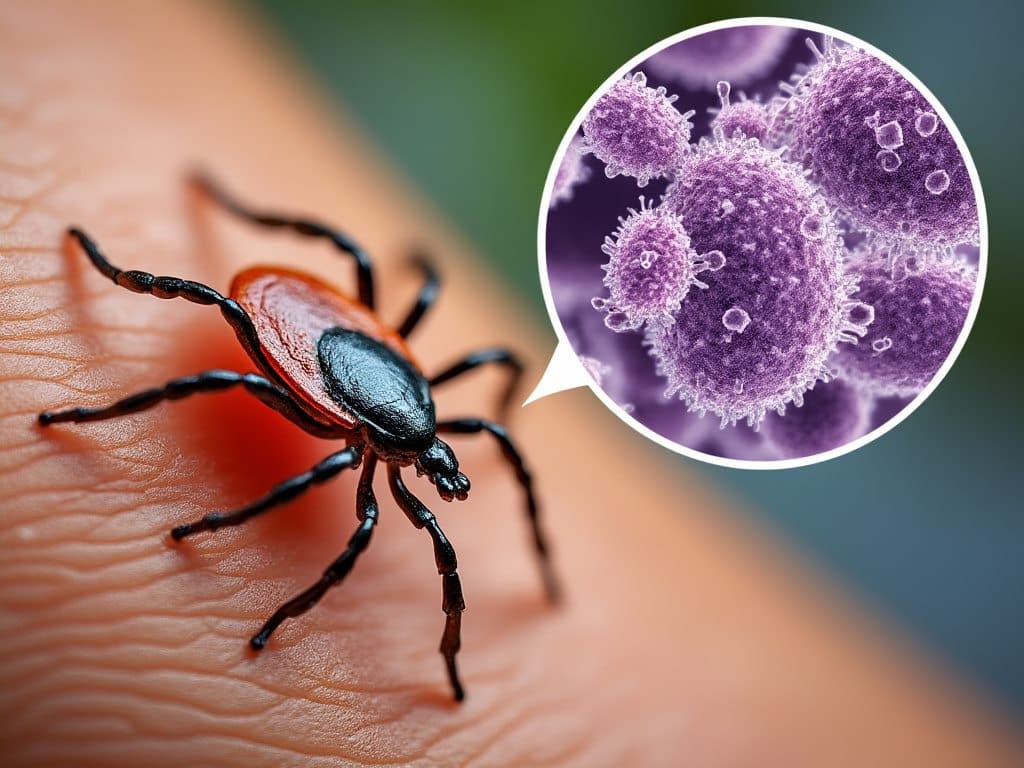
Diagnosing Lyme disease can be tricky. An ELISA test is usually the first step. It detects antibodies your body produces in response to the bacteria carried by ticks.
But relying solely on the ELISA test isn’t foolproof. Its accuracy can vary, and it is often paired with other Lyme Disease tests like the Western Blot to confirm results. Understanding the strengths and limitations of the ELISA test can help you navigate the complexities of Lyme disease diagnosis more effectively.
Key Takeaways
The ELISA (Enzyme-Linked Immunosorbent Assay) test for Lyme disease is a blood test designed to detect antibodies against Borrelia burgdorferi, the bacterium that causes Lyme disease. This test serves as the initial step in diagnosing Lyme disease.
The ELISA test screens for antibodies against B. burgdorferi. It doesn’t test for the bacteria but rather the immune response your body mounts to an infection by B. burgdorferi.
Positive Result: A positive ELISA result suggests antibodies, indicating a current or past infection. However, a positive result alone cannot confirm Lyme disease because false positives can occur. Further testing, typically involving the Western Blot test, is required to accurately verify the presence of Lyme disease.
You’ll first undergo a blood sample collection. This typically involves a healthcare professional inserting a needle into a vein in your arm to draw blood. It’s straightforward and usually takes just a few minutes.
Interestingly, no special preparation is needed for the ELISA test. You can eat, drink, and follow your regular routine before the test without any restrictions.
Once your blood sample is collected, it’s sent to a laboratory for analysis. Technicians will examine your blood at the lab for antibodies against Borrelia burgdorferi. They use the ELISA method to measure these antibody levels. The presence of antibodies indicates that your immune system has encountered the bacteria responsible for Lyme disease.
Lab personnel focus on detecting IgM and IgG antibodies. IgM antibodies, present in the early stages of Lyme disease, can provide early diagnostic insights. Conversely, IgG antibodies indicate later stages of infection, offering a broader diagnostic window. This meticulous analysis is important in understanding your infection’s progress and determining the appropriate next steps.
When preparing for the ELISA test for Lyme disease, no dietary restrictions are required, and no specific preparations are required.
The test procedure for Lyme disease involves taking a blood sample, where a healthcare professional will extract blood, typically in your arm. This quick process may cause moderate pain or a prick but is generally temporary. The blood sample is then sent to a laboratory where technicians analyze it for antibodies against Borrelia burgdorferi. IgM antibodies indicate early stages of infection, while IgG antibodies suggest a later stage. On the appointment day, wear easily rollable sleeves and stay well-hydrated to aid vein accessibility.
Do not worry if you’re uncertain about the test procedure—your healthcare professional will guide you through each step. It’s straightforward and doesn’t require extensive preparation.
When Lyme disease is suspected, the ELISA test serves as the initial testing.
Clinicians look for antibodies against Borrelia burgdorferi, the bacterium responsible for Lyme disease. This initial step helps determine if further testing is necessary.
The ELISA test measures antibodies in your blood, which form in response to the Lyme bacteria. Although it doesn’t detect the bacteria directly, it traces your immune system’s reaction, which indicates exposure to Borrelia burgdorferi. For example, detecting IgM antibodies suggests an early infection, while IgG antibodies indicate a later stage of infection.
While the ELISA test is sensitive and effectively detects antibodies, it has low specificity. This means it can produce false-positive results. To ensure accuracy, a positive ELISA test is usually confirmed with a second test, typically the Western blot. Without this confirmation, diagnostic errors might occur.
Clinicians rely on the ELISA test to make informed decisions about further diagnostic testing. If your ELISA test results are positive, doctors will likely order additional tests, like the Western blot, to confirm the diagnosis. This step is important for avoiding misdiagnosis and ensuring appropriate treatment.
Understanding the ELISA test results for Lyme disease is important for correct diagnosis and treatment. This section details normal and abnormal values, clarifying what these results mean.
A negative ELISA result signifies that no or very few antibodies to Lyme disease were detected in your blood sample. This generally means you don’t have Lyme disease, though it could also indicate an early-stage infection where antibodies have not yet developed. Typically, if the ELISA test is negative, no further testing is recommended unless you still have symptoms suggestive of Lyme disease.
A positive ELISA result indicates that antibodies against Borrelia burgdorferi, the bacterium causing Lyme disease, are in your blood. But, this result alone cannot confirm Lyme disease due to the potential for false positives. Hence, a confirmatory Western blot test is necessary if you have a positive or equivocal ELISA result. This step increases the specificity of the diagnosis, helping to rule out false positives and confirm whether you have Lyme disease.
The ELISA test offers high sensitivity, effectively detecting antibodies to Lyme disease. But, due to its low specificity, false-positive results can occur. In these instances, a Western blot test confirms the diagnosis. Hence, the ELISA test alone cannot definitively diagnose Lyme disease, requiring further testing.
False positives present a significant challenge with the ELISA test. Cross-reactivity with other microbes can generate antibodies that cause these incorrect results, leading to potential misdiagnosis. On the other hand, false negatives might occur early in the infection. Typically, the antibody response takes one to three weeks to develop, rendering early detection difficult. This delay in antibody production means that a negative ELISA test early on does not always rule out Lyme disease.
Sometimes, antibodies produced in response to other microbes cross-react with those for Lyme disease, causing false positives. So, it’s critical to consider these factors and rely on confirmation tests like the Western blot for accurate diagnosis.
The test’s good sensitivity can help catch the disease early, but because of its specificity issues, you need follow-up tests to avoid false positives.
Because you have likely had this disease for years or even decades, there is a likelihood that you will react to initial treatment strategies. As Borrelia dies, it will release its toxins. If you are in a chronic stage of Lyme Disease, Borrelia has likely disseminated throughout your body and made a home in many tissues. There will be a lot of microorganisms to kill and therefore a lot of toxins that will be released.
In order to properly treat chronic Lyme Disease symptoms, you will want to go slow and make sure your detoxification systems in your body are working properly for this. You can see our blog on Lyme Disease Treatment to learn more about this as well.
The ELISA test is a crucial first step for spotting antibodies against Borrelia burgdorferi. However, it has limitations, so you’ll need a follow-up like the Western Blot to nail down the diagnosis. Understanding the ins and outs of this test helps you make sense of the results and find the right treatment. Catching it early and getting a proper diagnosis is super important for managing Lyme disease. Consult a Lyme Literate Doctor for a comprehensive evaluation and follow-up testing for suspected Lyme disease.
References
DeLong, A., Hsu, M. & Kotsoris, H. Estimation of cumulative number of post-treatment Lyme disease cases in the US, 2016 and 2020. BMC Public Health 19, 352 (2019). https://doi.org/10.1186/s12889-019-6681-9
Schmid H, Heininger U. Posttreatment Lyme Disease Syndrome-What It Might Be and What It Is Not. Pediatr Infect Dis J. 2021 May 1;40(5S):S31-S34. doi: 10.1097/INF.0000000000002772. PMID: 34042908.
We have helped thousands of
people restore their health
and quality of life by diagnosing
and treating their Lyme Disease.
“Dr. Mueller’s approach to medicine is refreshing! There is only so much you can do with western medicine and in my life I was needing a new approach. By addressing the whole body, nutritional diet factors, environmental factors, blood work, and incorporating ideas I had not previously known, I was able to break through with my conditions. I am not only experiencing less pain in my life, but through the process of healing guided by Dr. Diane Mueller, I am now happy to say I have more consciousness surrounding how I eat, what to eat and when things are appropriate. Living by example Dr. Mueller has a vibrancy that makes you want to learn and know more about your body and overall health. I highly recommend her to anyone looking for new answers, a new approach to health, or in need of freedom from pain and limitations.”
-Storie S.
Kihei, HI
