
Written by Dr. Diane Mueller
Discovered in 1953 from Streptomyces hygroscopicus strains, hygromycin A is a fascinating antibiotic with a broad spectrum of activity against gram-positive and gram-negative bacteria. Unlike its structural cousin, hygromycin B, this compound inhibits ribosomal peptidyl transferase activity, blocking a critical step in bacterial protein synthesis.
Hygromycin A is an antibiotic discovered in 1953 from Streptomyces hygroscopicus that selectively targets spirochetes like Borrelia burgdorferi (Lyme disease) while sparing beneficial gut bacteria.
Unlike broad-spectrum antibiotics, hygromycin A inhibits ribosomal peptidyl transferase activity, specifically in spirochetes, offering precision treatment with minimal microbiome disruption.
Animal studies show hygromycin A cleared Lyme infections as effectively as traditional antibiotics, potentially reducing the risk of developing Post-Treatment Lyme Disease Syndrome.
Major limitations include lack of human clinical data, limited effectiveness against common Lyme co-infections, and uncertain activity against persister cells that may cause symptom recurrence.
Functional medicine approaches recommend integrating hygromycin A within a comprehensive protocol that includes gut health support, anti-inflammatory nutrition, and persister cells
Recent research has sparked renewed interest in hygromycin A due to its effectiveness in treating swine dysentery, a severe diarrheal disease in pigs. When added to feed at just 5-20 g/ton, it shows remarkable potency against Serpulina Treponema hyodysenteriae; the anaerobic spirochete believed to cause this condition. You’ll find it fascinating that scientists have developed over 100 analogs to determine their effectiveness, creating a comprehensive structure-activity relationship that reveals which molecular components are essential for their antibacterial properties.
Hygromycin A is a spirochete-specific antibiotic originally discovered in 1953 from a soil bacterium called Streptomyces hygroscopicus. Though initially overlooked for decades due to its weak activity against common pathogens, researchers have recently rediscovered its remarkable selective potency against spirochetes, particularly Borrelia burgdorferi – the bacterium responsible for Lyme disease.
Unlike broad-spectrum antibiotics currently used for Lyme treatment, Hygromycin A targets only the Lyme-causing bacteria precisely, leaving beneficial microbes untouched. This selectivity occurs by targeting bacterial ribosomes, disrupting protein synthesis specifically in spirochetes while sparing other bacterial species. What makes this compound especially interesting is that even though it has been known since the 1950s, its potential for treating Lyme disease has only recently come to light.
Hygromycin A stands out in the antibiotic world for its laser-focused action against Borrelia burgdorferi, the causative agent of Lyme disease. Unlike shotgun-approach antibiotics, it works with surgical precision by targeting specific bacterial mechanisms while leaving your beneficial gut bacteria largely untouched.
The magic happens at the ribosomal level—hygromycin A binds to bacterial ribosomes, effectively shutting down protein production in spirochetes. This binding mechanism blocks the peptidyl transferase activity, an important step for bacterial survival. This approach is particularly clever because hygromycin A exploits a unique transport system in Borrelia that other bacteria don’t share, creating its selective action.
MIce studies have delivered promising results, showing that hygromycin A successfully cleared Lyme infections, whether administered through injection or bait. The minimal impact on the microbiome is particularly significant considering that 10-20% of Lyme patients develop post-treatment Lyme disease syndrome (PTLDS), often linked to microbiome disruption from conventional antibiotics.
Doxycycline can contribute to the formation of these persistent cells. Studies have demonstrated that Borrelia adapts by altering its form to increase survival chances when exposed to the antibiotic.
This process complicates treatment, as the dormant cells may wait to resurface.
Hygromycin A’s narrow focus creates advantages and limitations compared to standard Lyme treatments. The targeted approach means less collateral damage to your gut microbiome, potentially reducing gastrointestinal side effects and lowering the risk of developing PTLDS.
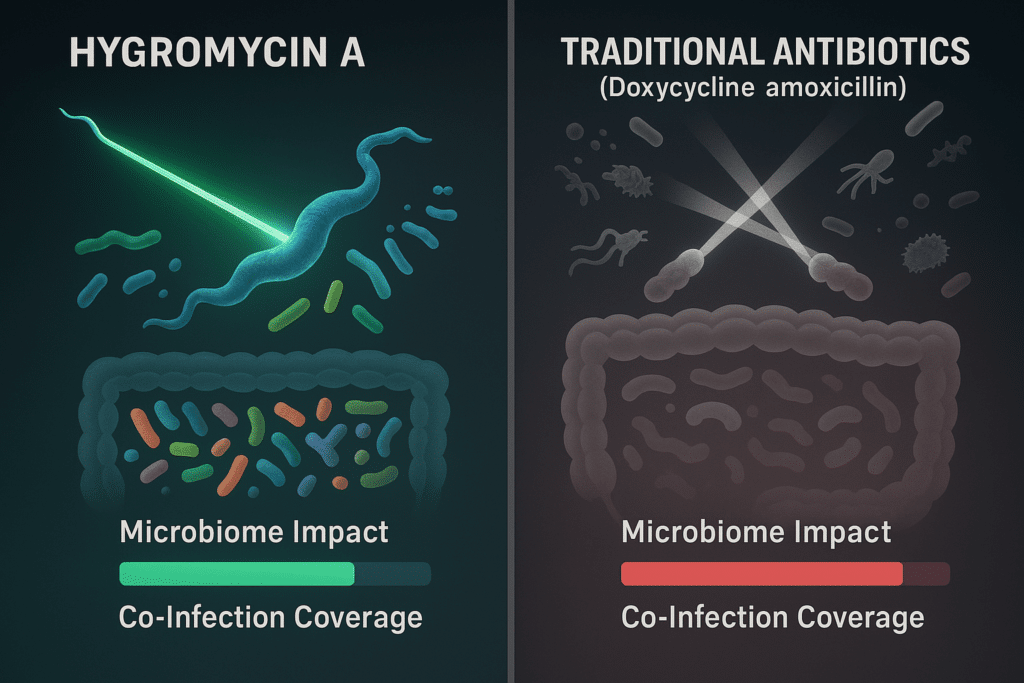
Antibiotic | Spectrum | Targets Lyme | Microbiome Impact | Co-Infection Coverage |
|---|---|---|---|---|
Hygromycin A | Narrow | Yes | Low | Limited |
Doxycycline | Broad | Yes | High | Yes |
Amoxicillin | Broad | Yes | High | Yes |
This selectivity has real-world implications. When taking traditional antibiotics like doxycycline or amoxicillin, patients often experience digestive issues as beneficial bacteria get caught in the crossfire. Hygromycin A’s targeted approach significantly reduces this problem.
The trade-off comes with co-infections. Many Lyme patients simultaneously battle additional tick-borne infections like Babesia or Bartonella. While traditional antibiotics may address multiple infections at once, hygromycin A’s specificity means these co-infections could remain untreated.
One of the toughest challenges in Lyme disease treatment is addressing persister cells—dormant Borrelia forms that evade antibiotics and later reactivate, often causing symptoms to return. While herbs like Cryptolepis sanguinolenta have shown promise against these stubborn cells in lab studies, there’s no solid evidence yet that hygromycin A can effectively target them.
This uncertainty raises critical questions about hygromycin A’s potential as a Lyme treatment. Can it fully eradicate the infection or merely suppress active bacteria, leaving persister cells untouched? Research is ongoing, but until clinical evidence emerges, this remains a key unanswered question for chronic Lyme patients seeking lasting relief.
Hygromycin A stands out in the antibiotic world for its remarkable ability to maintain gut flora integrity while fighting infection. Unlike conventional broad-spectrum antibiotics that indiscriminately destroy beneficial bacteria alongside pathogens, hygromycin A selectively targets Borrelia burgdorferi with minimal collateral damage to the microbiome.
Studies have demonstrated significantly less disruption to fecal microbiota composition with hygromycin A treatment than doxycycline (the current standard Lyme treatment). This preservation of gut flora represents a major win for doctors who recognize the microbiome as a cornerstone of overall health. The gut-brain connection, immune function, and inflammatory pathways depend on a balanced microbiome.
Hygromycin A’s unique mechanism of action offers promising resistance-fighting potential in the battle against Lyme disease. By targeting essential Borrelia transport systems through ribosomal peptidyl transferase inhibition, hygromycin A attacks the bacteria through pathways that provide fewer opportunities for adaptation.
Researchers theorize that this distinctive approach may slow the development of resistance, though long-term clinical data remain necessary to confirm this hypothesis. History reminds us to proceed with caution—previous “resistance-proof“ antibiotics eventually encountered adaptive bacterial strains as they gained widespread use.
For the approximately 20% of Lyme patients who develop persistent symptoms even through conventional treatment, hygromycin A represents a potential breakthrough. Its selective action against Borrelia combined with minimal microbiome disruption addresses two critical factors that may contribute to chronic Lyme symptoms.
While human trials are still pending, the medical community has noted growing anecdotal interest among patients who have exhausted conventional options. Hygromycin A’s true potential shines brightest when viewed not as a standalone solution but as part of an integrated protocol that includes targeted nutrition, detoxification support, immune modulation, and stress management.
Even though it has promising potential, hygromycin A has several important limitations that researchers and patients should be aware of when considering its use for Lyme disease treatment.
Hygromycin A’s effectiveness in humans remains theoretical, mainly as clinical studies are still early. While laboratory and animal studies show promise, the antibiotic hasn’t undergone rigorous human testing that would validate its safety and efficacy profiles.
Phase 1 Trials: Initial safety trials began in 2024, with preliminary results still pending
Extended Timeline: Full human efficacy trials aren’t expected to launch until 2026 or beyond
Unknown Factors: Potential side effects, optimal dosing, and efficacy in complex human cases remain undetermined
This gap in human data creates significant uncertainty about how hygromycin A might perform in real-world clinical settings, especially for patients with chronic or complicated Lyme infections.
Hygromycin A’s narrow targeting mechanism presents a notable drawback for comprehensive Lyme treatment. The antibiotic specifically targets spirochetes but shows limited activity against common Lyme co-infections.
Multiple Pathogens: Up to 40% of Lyme patients harbor co-infections like Babesia, Bartonella, or Anaplasma
Treatment Complexity: Patients with multiple infections may require additional antimicrobial agents alongside hygromycin A
Comprehensive Approach: Effective Lyme protocols often need to address the full spectrum of infections simultaneously
This limitation means hygromycin A would likely need to be part of a broader treatment strategy rather than a standalone solution for many Lyme patients.
Perhaps the most significant question surrounding hygromycin A is its effectiveness against persister cells—dormant forms of Borrelia that can survive traditional antibiotic treatment and potentially cause symptom recurrence.
Insufficient Evidence: Current research hasn’t conclusively demonstrated hygromycin A’s ability to eliminate persister forms of Borrelia
Critical Gap: Persister cells are implicated in treatment failures and development of chronic Lyme symptoms
Ongoing Questions: Whether hygromycin A can prevent relapses by targeting these dormant bacteria remains unknown
Functional medicine begins with thoroughly evaluating the patient’s unique health profile. Before considering Hygromycin A, practitioners assess:
Testing: Confirm Lyme and co-infections via specialized labs like GI-MAP or SpectraCell to establish a baseline understanding of infection status.
Symptoms: Evaluate the full spectrum of symptoms, including fatigue, pain patterns, cognitive issues, and gut health disruptions that may indicate spirochete infection.
History: Consider past antibiotic use and current microbiome status to determine how previous treatments affected gut flora integrity.
If Hygromycin A is deemed appropriate, it’s integrated into a broader protocol that addresses both the infection and underlying health factors:
Antimicrobial Support: Pair with herbs like Japanese knotweed that target persister cells and biofilms that Hygromycin A alone might miss.
Nutrition: Carry out an anti-inflammatory diet (e.g., Mediterranean) rich in polyphenols and omega-3s to reduce systemic inflammation and support immune function.
Supplements: Add targeted probiotics, vitamin D, and omega-3s to support immunity and maintain microbiome diversity during treatment.
Component | Purpose | Example |
|---|---|---|
Antibiotic | Target Borrelia | Hygromycin A (if available) |
Herbal Support | Address persister cells, co-infections | Cryptolepis, Artemisia |
Nutrition | Reduce inflammation | Mediterranean diet |
Supplements | Boost immunity, gut health | Probiotics, vitamin D |
Functional medicine emphasizes holistic healing beyond antimicrobials, addressing stress, sleep, and movement patterns to enhance recovery:
Stress Management: Incorporate daily meditation or yoga practices to lower cortisol levels that can suppress immune function and worsen inflammation.
Sleep Hygiene: Prioritize 7-9 hours of quality sleep to support immune repair and natural detoxification processes essential during treatment.
Exercise: Engage in gentle movement like walking or swimming to improve lymphatic circulation without triggering post-exertional malaise common in Lyme patients.
Labs: Reassess microbiome diversity and inflammatory markers to confirm Hygromycin A works without disrupting gut flora.
Symptom Tracking: Adjust therapies based on changes in fatigue, pain levels, or cognitive function using validated symptom scales.
Collaboration: Work with Lyme-literate doctors for Hygromycin A access and integration with conventional medicine approaches when necessary.
Hygromycin A was discovered in 1953 from Streptomyces hygroscopicus strains. It has broad-spectrum activity against both gram-positive and gram-negative bacteria. It works by inhibiting ribosomal peptidyl transferase activity, which blocks bacterial protein synthesis. Unlike other antibiotics, hygromycin A selectively targets spirochetes while preserving beneficial gut microbes, making it particularly interesting for Lyme disease treatment.
Hygromycin A binds to bacterial ribosomes and shuts down protein production, specifically in spirochetes like Borrelia burgdorferi, the bacterium causing Lyme disease. This targeted mechanism allows it to kill the infection while minimizing impact on the gut microbiome. This selectivity is valuable because traditional antibiotics often disrupt beneficial gut bacteria, which may contribute to post-treatment Lyme disease syndrome in 10-20% of patients.
Hygromycin A is still in the early research phases for human use. Initial safety trials are expected to begin in 2024, with full efficacy trials not anticipated until 2026 or later. It’s not FDA-approved, which means it could take several years before becoming commercially available as a treatment option. Patients interested in this treatment should monitor clinical trial developments.
The effectiveness of hygromycin A against persister cells (dormant forms of Borrelia that can evade treatment) remains uncertain. Research is ongoing to determine whether it can eliminate these treatment-resistant bacteria that often cause symptom recurrence. Until definitive evidence emerges, clinicians may need to combine hygromycin A with other agents specifically targeting persister cells as part of a comprehensive treatment approach.
No, hygromycin A specifically targets spirochetes like Borrelia burgdorferi but may not address common Lyme co-infections such as Babesia or Bartonella. Its narrow targeting mechanism limits its effectiveness as a standalone treatment for patients with multiple tick-borne infections. Those suspected co-infections would likely need additional antimicrobial therapies alongside hygromycin A for comprehensive treatment.
Unlike broad-spectrum antibiotics like doxycycline, hygromycin A selectively targets spirochetes while preserving beneficial gut bacteria. Mouse studies show it causes significantly less disruption to fecal microbiota than traditional treatments. This selectivity may reduce gastrointestinal side effects, decrease the risk of antibiotic resistance, and lower the likelihood of developing post-treatment Lyme disease syndrome.
Hygromycin A represents a promising frontier in Lyme disease treatment. With its targeted approach to eliminating Borrelia while preserving gut health, this selective antibiotic offers hope, particularly for those struggling with persistent symptoms or microbiome disruption from conventional treatments.
The road ahead includes critical human trials beginning in 2024 that will determine its actual effectiveness and safety profile. Until then, it remains an intriguing but unproven option.
For optimal results, you’ll need to view hygromycin A as just one component of a comprehensive treatment strategy that addresses co-infections, persister cells, and underlying immune dysfunction. Working with a Lyme Literate practitioner who can integrate this potential new treatment option within a personalized protocol will be essential to your healing journey.
Arnaboldi, P., & Narasimhan, S. (2021). Hygromycin A in the Lymelight.. Cell host & microbe, 29 11, 1599-1601 . https://doi.org/10.1016/j.chom.2021.10.007.
Feng, J., & Zhang, Y. (2018). Proteomic Analyses of Morphological Variants of Borrelia burgdorferi Shed New Light on Persistence Mechanisms: Implications for Pathogenesis, Diagnosis and Treatment. bioRxiv. https://doi.org/10.1101/501080.
We have helped thousands of
people restore their health
and quality of life by diagnosing
and treating their Lyme Disease.
“Dr. Mueller’s approach to medicine is refreshing! There is only so much you can do with western medicine and in my life I was needing a new approach. By addressing the whole body, nutritional diet factors, environmental factors, blood work, and incorporating ideas I had not previously known, I was able to break through with my conditions. I am not only experiencing less pain in my life, but through the process of healing guided by Dr. Diane Mueller, I am now happy to say I have more consciousness surrounding how I eat, what to eat and when things are appropriate. Living by example Dr. Mueller has a vibrancy that makes you want to learn and know more about your body and overall health. I highly recommend her to anyone looking for new answers, a new approach to health, or in need of freedom from pain and limitations.”
-Storie S.
Kihei, HI
