
Written by Dr. Diane Mueller
Ever felt nauseous in your home or office for no discernible reason? You might not have considered that your environment could make you ill, potentially with mold. Mold and its more lethal cousin, mildew, don’t just compromise structures and materials; they can also compromise your health. And nausea is one of the most commonly reported symptoms.
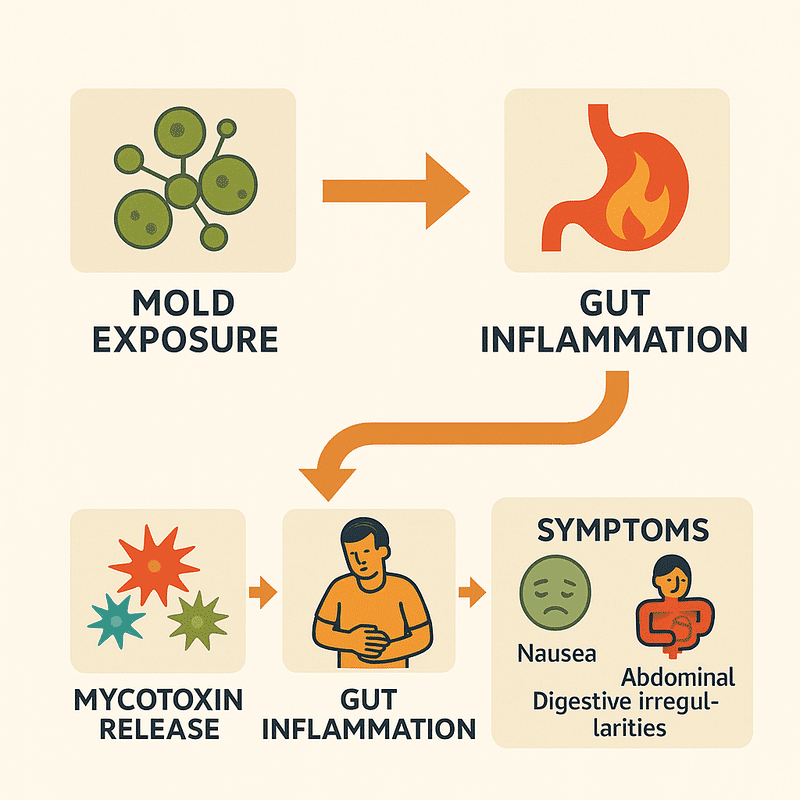
Mold exposure can cause nausea and digestive symptoms, not just respiratory issues, as toxic mycotoxins can irritate the gastrointestinal lining and disrupt normal digestive processes.
Standard medical evaluations often miss the connection between persistent nausea and environmental triggers like mold, leading to symptom-based treatments rather than addressing the root cause.
Common symptoms of mold-related digestive issues include persistent nausea that comes and goes, unexplained abdominal pain, digestive irregularities, and loss of appetite.
Before concluding that mold is causing your nausea, rule out other “horses” (common causes) such as poor diet, dehydration, parasites, fungal overgrowth, bacterial imbalances, and digestive enzyme deficiencies.
Treating only the symptoms of mold exposure with medications can create an illusion of wellness while allowing underlying systemic inflammation to continue, potentially leading to new health problems.
When mold spores are in your living or working environment, they can trigger various reactions. While many people associate mold with respiratory issues like coughing or wheezing, its connection to digestive symptoms, particularly nausea, is less commonly discussed yet equally important to understand.
Digestive symptoms like nausea, abdominal pain, constipation, and diarrhea can signal underlying health issues. While often linked to food or stress, these issues can also result from environmental factors like mold exposure. Mold is commonly known for causing respiratory problems, but it can also lead to persistent digestive distress, especially in specific environments. Identifying mold exposure as a potential cause can help address the root issue rather than just managing symptoms, even if standard medical tests fail to find an explanation.
We have helped thousands of people restore their health and quality of life by diagnosing and treating their Mold Illness.
Understanding the root causes of health issues is essential for effective treatment, especially when dealing with symptoms like nausea that could be related to mold exposure.
Standard medical evaluations often fall short when identifying environmental triggers like mold. Many conventional tests focus on ruling out severe conditions rather than finding the underlying cause of symptoms. Blood work, endoscopies, and imaging studies can appear normal even when experiencing significant digestive distress from mold exposure.
Doctors typically aren’t trained to look for environmental toxins and may not connect your recurring nausea to potential mold in your home or workplace. This gap in assessment can leave you cycling through treatments that address your symptoms without resolving the real problem. Also, insurance-driven healthcare often limits physicians’ time to investigate complex environmental health connections thoroughly.
Many patients find themselves in a frustrating situation where doctors say, “We don’t know the cause,“ and apply generic labels like IBS (Irritable Bowel Syndrome). Even when diagnosed with more specific conditions like ulcerative colitis, Crohn’s disease, or gastric emptying syndrome, these labels describe the condition but don’t explain why it developed.
This approach misses an important point—your body doesn’t randomly manifest disease. You’re only getting part of the picture when you receive diagnoses like these without exploring potential environmental triggers such as mold exposure. These diagnostic labels, while medically valid, often function as descriptive terms rather than explanations, leaving the underlying cause, which could be mold toxicity, unaddressed and continuing to trigger your nausea and other digestive symptoms.
Disease doesn’t simply appear out of nowhere—it develops through a complex interplay of factors that affect our body systems over time.
Mold-induced nausea is usually palliatively treated with symptom management. Meds for nausea may offer momentary relief, but they don’t do anything about the real problem: the harmful mold you’re still breathing in. Not addressing the cause can place both your health and your sense of well-being in jeopardy, leading to what might feel like a false improvement. Most diagnosis procedures for mold-related illnesses can take weeks or months to yield results, so it’s easy to understand how some might slip into the cycle of feel-better hopes followed by returns to troublesome symptoms. Without treating the cause, some patients might feel caught in a Health Care Speakeasy.
Asking “why” you’re experiencing nausea changes everything about how you approach treatment. Instead of just wondering how to stop feeling sick, you start investigating what’s making you sick in the first place. In medicine, there’s a saying: “If you hear hooves, think horses, not zebras.“ This means doctors typically look for common explanations before rare ones. But when it comes to persistent nausea, environmental factors like mold exposure are often overlooked, even though they are relatively common.
When you begin questioning why your symptoms persist despite treatment, you open the door to discovering environmental triggers that conventional approaches might miss. This curiosity-driven approach helps you connect seemingly unrelated symptoms, like why you feel better when you’re away from home or why multiple family members experience different health issues simultaneously.
Digging deeper into the “why” behind your symptoms often reveals patterns that point to specific causes. For example, mold exposure becomes a more likely culprit if your nausea worsens after rainy periods or in certain rooms of your house. This investigative mindset empowers you to take control of your health journey rather than passively receiving treatments that only address the surface problem.
Mold exposure represents an often overlooked cause of digestive issues, particularly nausea and abdominal discomfort. While many healthcare providers focus primarily on respiratory symptoms when discussing mold exposure, emerging research confirms that digestive manifestations can be equally problematic for affected individuals.
Mycotoxins—toxic compounds that particular mold species produce—can directly trigger digestive distress. Clinical observations and research studies have demonstrated that these toxins don’t just affect your respiratory system; they can cause significant gastrointestinal symptoms, including:
Persistent nausea that comes and goes without apparent cause
Unexplained abdominal pain and cramping
Digestive irregularities that don’t respond to conventional treatments
Loss of appetite and associated weight changes
The relationship between mold toxins and nausea isn’t merely theoretical. Research has identified that mycotoxins can irritate the gastrointestinal lining, disrupt normal digestive processes, and even impact your gut microbiome, potentially leading to chronic digestive complaints that might be misdiagnosed as other conditions.
Have Mold Illness or suspect you do?
We have helped thousands of people restore their health and quality of life by diagnosing and treating their Mold Illness.
Before concluding that mold is the culprit behind your digestive distress, it’s essential to investigate other potential causes contributing to or mimicking mold-related symptoms.
A comprehensive digestive health assessment should include:
Parasite screening: Many parasitic infections cause nausea and digestive upset. Importantly, not all parasites show up on standard tests, making them easy to miss in routine examinations.
Fungal overgrowth evaluation: Candida and another fungal overgrowths in your digestive tract can produce symptoms similar to mold exposure, including persistent nausea and abdominal discomfort.
Small Intestinal Bacterial Overgrowth (SIBO) testing: When bacteria that usually reside in your large intestine migrate and proliferate in your small intestine, they can cause significant digestive disturbances, including nausea, bloating, and irregular bowel movements.
Stomach acid assessment: Insufficient stomach acid (hypochlorhydria) can lead to poor digestion, nutrient malabsorption, and chronic nausea—symptoms that might be incorrectly attributed to other causes.
Pancreatic enzyme function: Inadequate production of digestive enzymes from your pancreas can result in poor breakdown of food, leading to nausea and other digestive complaints.
These underlying digestive issues often operate alongside environmental exposures, creating complex clinical pictures that require thorough investigation. Addressing environmental triggers (like mold) and these digestive factors provides the most comprehensive approach to resolving persistent nausea and related symptoms.
Receiving a diagnosis of anything, including digestive issues, should be the starting point for developing a deeper understanding of oneself and not the endpoint.
Nausea that won’t go away may have some hidden reason like mold exposure, which can easily be brushed off.
Gastritis or dyspepsia might describe the symptoms but don’t explain the root cause.
Further investigation is essential, particularly when mold toxicity might be a concealed contributing factor.
The typical medical approach often addresses symptoms like mold-related nausea with medications that provide temporary relief, without investigating the underlying cause. This can leave mold exposure and its effects unaddressed.
To tackle the issue, it’s essential to look beyond symptom management and explore the root cause, such as mycotoxins from mold, for a more effective and lasting solution.
Mold exposure can cause nausea by triggering systemic inflammation in the body. Treating only the symptoms, like nausea, may provide temporary relief, but it doesn’t stop the underlying inflammation.
This inflammation spreads to multiple organ systems, affecting the nervous system, respiratory tract, and skin. Mold toxins continue circulating in your bloodstream, causing widespread inflammatory responses even if immediate symptoms seem to improve.
Ignoring the root cause of nausea caused by mold exposure can lead to ongoing health problems. Staying in a contaminated environment allows harmful mycotoxins to build up, resulting in new symptoms like fatigue, brain fog, skin rashes, or respiratory issues. Treating these symptoms separately without addressing the mold exposure can lead to multiple diagnoses, medications, and side effects, creating a cycle of unresolved health problems.
Rather than continuing this cycle, addressing the source of inflammation—removing yourself from mold exposure and supporting your body’s detoxification processes—provides the foundation for proper healing.
Yes, mold exposure can cause digestive problems, including nausea, abdominal pain, diarrhea, and constipation. Mycotoxins produced by particular mold species can irritate the gastrointestinal lining and disrupt normal digestive processes. These symptoms often persist despite conventional treatments and may be misdiagnosed as other conditions, like IBS, when the true culprit is environmental mold exposure.
Doctors often miss mold as a cause of digestive issues because conventional medical training focuses on ruling out severe conditions rather than investigating environmental factors. Many physicians are not adequately trained to recognize environmental toxicity. Standard testing doesn’t typically include screening for mold exposure, leading to generic diagnoses like IBS without identifying the actual root cause of symptoms.
Consider whether your symptoms worsen in certain environments (home, office, basement) or improve when you’re away. Look for visible mold or water damage in your living spaces. Track whether symptoms correlate with rainy weather or high humidity. If conventional treatments haven’t helped and you’ve been diagnosed with IBS without a clear cause, mold exposure could be worth investigating, especially if you also experience respiratory issues or fatigue.
If you suspect mold is causing your digestive symptoms, identify and address potential mold sources in your environment. Consider consulting with an environmental medicine specialist or functional medicine doctor experienced with mold-related illness. Professional mold inspection of your home or workplace may be necessary. Support your body’s natural detoxification processes and temporarily relocate to see if symptoms improve in a different environment.
Treating just the digestive symptoms without addressing the underlying mold exposure creates a false sense of wellness while allowing systemic inflammation to continue. This approach may temporarily mask symptoms but won’t resolve the root cause. Over time, inflammation can spread to other organ systems, creating new symptoms and health problems. Complete recovery typically requires removing the source of mold exposure.
Mold exposure leads to systemic inflammation when mycotoxins enter the bloodstream, triggering an immune response. These toxins can damage cell membranes, disrupt cellular function, and promote oxidative stress. The body’s attempt to neutralize these toxins creates inflammatory cascades that can affect multiple organ systems, not just the digestive tract. This explains why mold exposure often causes diverse symptoms beyond digestion.
Mold exposure can trigger nausea and other digestive issues through the harmful mycotoxins certain molds produce. When you’re experiencing persistent digestive symptoms that don’t respond to conventional treatments, it’s worth investigating your environment for mold contamination.
Don’t settle for symptom management alone. True healing requires identifying and addressing the root cause of your health concerns. This might mean testing your home or workplace for mold, examining your diet, or consulting a doctor who recognizes environmental illness.
Kolmodin-Hedman, B., Blomquist, G., & Sikström, E. (1986). Mould exposure in museum personnel. International Archives of Occupational and Environmental Health, 57, 321-323. https://doi.org/10.1007/BF00406187.
Weinstock, L., Campbell, A., Curtis, L., & Gutovich, J. (2024). Mycotoxin-Triggered Attacks of Nausea, Vomiting, and Abdominal Pain and Episodes of Pseudo-Obstruction. Universal Library of Medical and Health Sciences. https://doi.org/10.70315/uloap.ulmhs.2024.0201008.
We have helped thousands of
people restore their health
and quality of life by diagnosing
and treating their Lyme Disease.
“Dr. Mueller’s approach to medicine is refreshing! There is only so much you can do with western medicine and in my life I was needing a new approach. By addressing the whole body, nutritional diet factors, environmental factors, blood work, and incorporating ideas I had not previously known, I was able to break through with my conditions. I am not only experiencing less pain in my life, but through the process of healing guided by Dr. Diane Mueller, I am now happy to say I have more consciousness surrounding how I eat, what to eat and when things are appropriate. Living by example Dr. Mueller has a vibrancy that makes you want to learn and know more about your body and overall health. I highly recommend her to anyone looking for new answers, a new approach to health, or in need of freedom from pain and limitations.”
-Storie S.
Kihei, HI
