
Written by Dr. Diane Mueller
Have you ever noticed an unusual rash and wondered if it’s just a bug bite or something more serious? Spotting a red ring on your arm could be the Lyme Disease bullseye rash. Contrary to popular belief, Lyme disease isn’t limited to remote forests; it’s increasingly found in suburban areas and parks across the U.S., including relative dry areas like the Colorado Rockies.
The Lyme disease bullseye rash, also known as erythema migrans, appears in only about one-third of cases and does not always have the classic target-like appearance.
Rashes can vary in shape, color, and location, and may sometimes be absent, making diagnosis based on rash alone unreliable.
Additional flu-like symptoms such as fatigue, joint pain, and fever often occur with or without the rash, so monitoring your overall health after a tick bite is essential.
Diagnosis of Lyme disease can be challenging; initial blood tests may miss early infections, so keeping photos and notes about rashes and symptoms can help your healthcare provider.
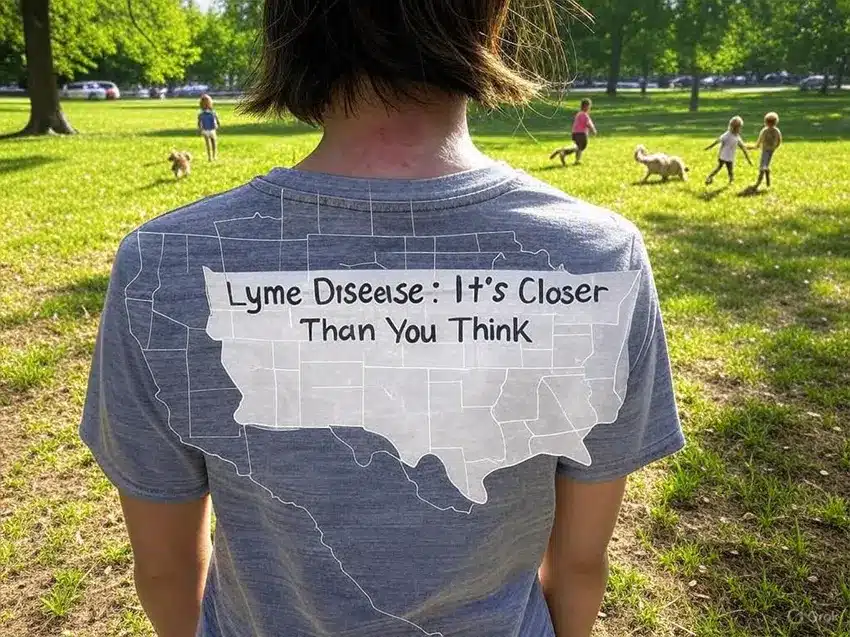
Lyme disease is found across the United States, not just in the Northeast, so vigilance is essential wherever ticks are present.
Early detection and seeking medical advice if you suspect Lyme disease is crucial to prevent chronic complications.
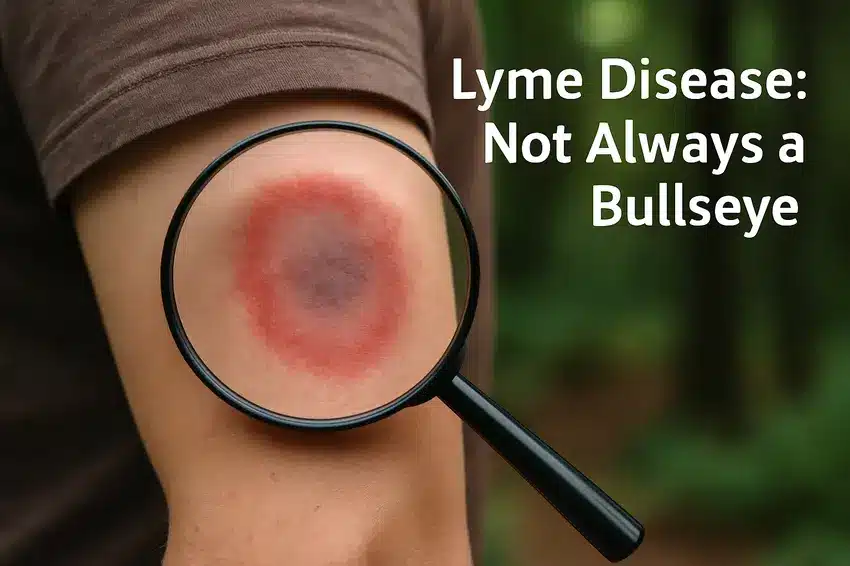
The rash can appear in different forms, such as a circular pattern, an irregular oval, or even with unclear edges.
Recognizing these variations is crucial. This article explores the bullseye rash, its importance, and the steps to take if you find one.
Lyme Disease Rash Myth Busters
If you’re like a lot of folks, you grew up thinking the “bullseye rash” was Lyme disease’s neon sign. The problem is that reality is wily—a chameleon who likes to keep things interesting (and a little confusing). Let’s dig into the most stubborn myths you’ll hear in the wild—and what you must watch for.
Myth 1: The Erythema Migrans Rash Always Resembles a Classic Bullseye
Here’s the biggie. You spot a red patch—no bullseye, just a warmish pink blob—and shrug it off, right? Hold up. Most Lyme disease rashes aren’t perfect textbook targets. Some skip the rings entirely. Instead, you might see a plain, round, or oval reddish patch, sometimes bluish or purplish, that grows like a slow-moving ripple on a pond. I’ve seen folks ignore a “boring” red rash to fight bigger headaches down the road. Don’t play detective if it spreads, feels warm, or looks odd. Snap a photo, note the date, and get a pro’s opinion.
This myth is one I fell for after a camping trip in Vermont (spoiler alert: ticks don’t care about state lines—or personal space). Multiple rashes can pop up, as if the bacteria decided to host a neighborhood block party across your skin. So if you notice more than one weird patch—even if only one bite is obvious—you’re not imagining things. Lyme can play hopscotch with your body.
You’ll hear, “Everyone with Lyme gets that rash,” tossed around all summer. Nope. Maybe one out of three people gets the classic skin sign. I know—a third isn’t everyone, no matter how you slice it. So, don’t count yourself out if you’re feverish, achy, and rash-free. Early Lyme is a master of disguise—trust symptoms, not stereotypes.
That’s wishful thinking—and trust me, I wish it were true too. Lyme doesn’t RSVP with a rash every time. Sometimes, symptoms like fatigue or joint pain show up without the fanfare of skin changes. If you’ve been in tick territory lately, don’t let the absence of a “badge” lull you. Your body might be fighting its own private battle.
You yank out a tick, stare anxiously for a day or two, then breathe easy when nothing appears. But Lyme rashes are the slowpoke of the skin eruption world. They might take anywhere from 3 to 30 days before entering, sometimes over a week before the drama unfolds. I’ve seen friends convinced they were in the clear, only to be surprised days later by a spreading mark.
Suppose you’re picturing a sting or burn, like those cartoon rashes with zippy zigzags, not so fast. The Lyme rash usually feels like…well, nothing much. Maybe a little warm, perhaps some faint tingling, but rarely stinging or throbbing. It’s sneaky quiet—no fireworks, no screaming pain. That’s why it’s so easy to miss. I’ve checked countless rashes, and sometimes even the person with it barely notices until it’s grown.
Scratch that—pun completely intended. Some rashes itch, but Lyme isn’t usually one of them. You might get mild itchiness, but far more common is a subtle redness that doesn’t cry out for a back scratcher. Seriously, I once compared notes with a friend who thought she’d brushed up against poison ivy—turned out to be Lyme, minus the urge to itch.
This is where Lyme likes to layer on the confusion. The rash isn’t the only sign—about half of the people will also feel flu-like (achy, tired, possibly a bit cranky). I remember a friend who thought her summer cold was just allergies until a rash cropped up. Think of the rash as the (sometimes missing) cover art on an album of vague symptoms. Headache, joint pain, and fever may arrive first, with the rash coming late.
Whenever you spot something weird after a walk in the woods—or your dog drags home an unwanted hitchhiker—snap close-up pics, jot down dates, and track any other strange feelings. Rashes can be sneaky, but your phone’s camera might be your new best friend for nabbing details before they fade.
At our medical clinic, most of the people that we find positive for Lyme Disease through testing do not remember a tick bit or ever having the classic Lyme Disease Rash.
If you’ve ever found yourself staring at a weird rash—maybe it’s a splotchy circle or a classic “bullseye”—then you know that sinking feeling. Lyme disease loves to keep folks guessing, never showing up quite the same way twice. Understanding the key facts and knowing what to look for offers armor against feeling lost in the tick-borne woods.
Let’s get one thing straight: spotting Lyme disease isn’t as apparent as waiting for a bright red target to bloom on your skin. Sure, you’ve heard about the “bullseye” rash, but only about a third of people with Lyme (think, one out of three) ever get that telltale mark. Now imagine the rash lurking somewhere sneaky, hidden under your hairline or behind your knee. Suddenly, playing bathroom-mirror detective becomes a lot less fun.
Underdiagnosis is common because many people (and let’s be honest, sometimes doctors) believe if there’s no iconic rash, there’s no Lyme. The real world is way messier. The bacteria responsible for Lyme don’t always leave calling cards. And those blood tests you hope will give a simple yes or no? They can miss early Lyme entirely. Picture this: your friend’s rash popped up behind their ear, out of sight, out of mind, and their bloodwork said nothing was wrong. The adventure to find answers started long after that tick had its fill.
Sometimes, Lyme shows up dressed as the world’s most annoying flu: fever, chills, stabbing headaches, sore muscles, and swamped-with-exhaustion days. Sound familiar? It’s like your body inflates a “closed for business” sign and refuses to open up shop.
Here’s a curveball—those symptoms might waltz whether you ever had a rash. More than one neighbor has chalked it up to a summer bug, only for the aches and brain fog to stick around. If left alone, Lyme can morph into a real life-changer: aching joints that seem to nag for months, full-body fatigue that doesn’t shake off, or the weirdest migraines you’ve ever felt. Some folks I know have spent months thinking they work too much, only to discover the root was a tiny tick bite and a rash they never noticed.
If you think you must be camping in the forests of Connecticut or trudging across grassy Vermont trails to get Lyme disease, let’s pump the brakes right there. Lyme isn’t picky about zip codes. Maybe you picked up the culprit at a Texas BBQ, or in your backyard in California. Ticks, it turns out, don’t care about state lines or city limits. They’ll hitch a ride with deer, pets, or even your shoes, and they’re making themselves right at home everywhere from city parks to suburban lawns.
The idea that the famed “bullseye” rash only strikes in New England or far-flung rural counties is just a story we tell ourselves. Friends get bitten at outdoor concerts in open fields, picnics, or raking leaves. Lyme is global—the bacteria and their spotted friends, black-legged ticks, know how to travel.
Rash Feature | How Often? | Where It Might Show Up | What It Looks Like |
|---|---|---|---|
Classic bullseye (target) | ~33% of cases | Trunk, armpit, thighs | Red ring with central clearing |
Plain red/blue patch | More common overall | Scalp, behind knees, ears | Solid color, sometimes bluish |
Multiple rashes | Occasionally | Various parts of the body | Small ovals, circles, or clustered |
No rash at all | Frequently (~67%) | — | — |
So, if something on your skin doesn’t feel right, or the “flu” you caught seems to have set up permanent residence, trust your instincts. Lyme disease can be a master of disguise—but now you know some of its favorite tricks.
Lyme disease isn’t just a blip on your summer radar—it can turn into a chronic, shape-shifting puzzle. That bullseye rash might seem straightforward, but sometimes, the aftermath is way messier than anyone bargained for. Ever felt like a health mystery, with symptoms popping up long after you swatted a bug away? Lyme’s got a knack for rewriting the plot, especially when your immune and hormonal systems start acting like mismatched socks—one pulling this way, one tugging that way.
Testing for Lyme disease can be unreliable. The standard two-tier testing misses infections up to 67% of the time, giving false negatives to many. The Western Blot test focuses on just one type of Lyme-causing bacteria, ignoring other related strains that can also cause the rash. For example, a friend with the classic bullseye rash tested negative but developed symptoms like joint pain and brain fog months later. If symptoms persist despite negative tests, consider advanced or repeat testing and keep a symptom diary for better tracking.
Feeling lost in medical jargon? Dr. Diane’s book It’s Not in Your Mind is a straightforward guide to chronic illness and puzzling symptoms like skin issues. For quick insights, check out our Get Well Quiz to suggest next steps.
Looking for community? Join our group program led by those who understand Lyme disease, sharing advice and lessons learned. Remember, you’re not alone—use these resources, keep asking questions, and persist until you find answers.
Trusting your instincts and staying vigilant about any unusual symptoms after a tick bite can make a real difference in your health. Don’t hesitate to seek medical advice and push for answers if you notice a rash or feel unwell, without classic signs.
Your documentation and persistence are key tools in getting the correct diagnosis. Remember, Lyme disease is often misunderstood and can present in many ways, so being proactive is your best defense. Stay informed and advocate for your well-being.
Erythema migrans is the distinctive bullseye rash that appears after a tick bite in people infected with Lyme disease. It’s critically important because it occurs in 70-80% of infected individuals and is a key early indicator of Lyme disease infection. Recognizing this rash allows for prompt medical intervention, significantly improving treatment outcomes before the infection progresses to more serious stages.
The Lyme disease rash typically develops between 3 and 30 days after an infected tick bite. It starts small at the bite location and gradually expands over days or weeks, often reaching several inches in diameter. The expanding nature of the rash is a distinctive characteristic that helps differentiate it from other skin conditions or reactions.
The Lyme disease rash doesn’t always present as the classic bullseye pattern. While the target-like appearance with a clear center is typical, the rash can also appear as a solid red patch, have multiple rings, or present with varying shapes and colors. This variation often leads to missed diagnoses when people expect only the classic bullseye presentation.
Approximately 20-30% of people with Lyme disease never develop the characteristic rash. The absence of a rash doesn’t rule out infection, so it’s essential to be aware of other symptoms like fever, fatigue, headache, and joint pain. Anyone with these symptoms who has been in tick-prone areas should consult a healthcare provider regardless of whether a rash appeared.
Lyme disease is frequently misdiagnosed because its symptoms mimic many other conditions, like the flu, fibromyalgia, or chronic fatigue syndrome. Additionally, standard blood tests have high false-negative rates, especially in early infection stages. The misconception that all cases present with a bullseye rash and that many rashes go unnoticed in hidden body areas further complicates accurate diagnosis.
Untreated Lyme disease can lead to serious long-term health issues, including chronic joint inflammation (particularly in the knees), neurological complications like Bell’s palsy and meningitis, cognitive problems, heart rhythm abnormalities, and persistent fatigue. These complications can develop months or even years after the initial infection, making the connection to Lyme disease difficult to establish.
No, Lyme disease is not limited to New England. While initially associated with the Northeast United States, it’s now recognized as a global health concern. Cases across North America, Europe, Asia, and Australia have been documented. Climate change and urban development have expanded tick habitats, increasing human exposure risk in many regions previously considered low-risk.
Murray TS, Shapiro ED. Lyme disease. Clin Lab Med. 2010 Mar;30(1):311-28. doi: 10.1016/j.cll.2010.01.003. PMID: 20513553; PMCID: PMC3652387.
Skar GL, Blum MA, Simonsen KA. Lyme Disease. [Updated 2024 Oct 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431066/
We have helped thousands of
people restore their health
and quality of life by diagnosing
and treating their Lyme Disease.
“Dr. Mueller’s approach to medicine is refreshing! There is only so much you can do with western medicine and in my life I was needing a new approach. By addressing the whole body, nutritional diet factors, environmental factors, blood work, and incorporating ideas I had not previously known, I was able to break through with my conditions. I am not only experiencing less pain in my life, but through the process of healing guided by Dr. Diane Mueller, I am now happy to say I have more consciousness surrounding how I eat, what to eat and when things are appropriate. Living by example Dr. Mueller has a vibrancy that makes you want to learn and know more about your body and overall health. I highly recommend her to anyone looking for new answers, a new approach to health, or in need of freedom from pain and limitations.”
-Storie S.
Kihei, HI
