
Written by Dr. Diane Mueller
Battling Lyme disease for months or even years without relief isn’t just frustrating—it’s a reality for the 20% of patients who find lyme disease treatments do not work. When antibiotics and standard protocols leave you still exhausted and in pain, it’s not a sign to give up, but rather to look deeper at the often-overlooked factors like co-infections, mold exposure, and immune dysfunction that might be sabotaging your recovery.
Isn’t it time to explore why your current Lyme treatment plan is falling short and discover the alternative approaches that could finally help you reclaim your health?
Conventional Lyme treatments fail up to 20% of patients due to unaddressed underlying factors like co-infections, mold toxicity, and immune dysfunction that standard antibiotic protocols don’t target
Multiple hidden conditions often masquerade as treatment-resistant Lyme, including toxic mold exposure, bacterial co-infections like Babesia and Bartonella, and cellular damage that persists even after successful bacteria elimination
Comprehensive testing beyond standard Lyme panels is essential for identifying root causes, including mycotoxin tests, co-infection panels, mitochondrial function assessments, and screening for hidden infections like C. diff and MARCoNS
A systematic approach addressing all identified issues simultaneously produces better outcomes than targeting Lyme bacteria alone, requiring detoxification support, environmental changes, and cellular repair protocols
Recovery requires partnering with Lyme-literate or functional medicine practitioners who understand complex chronic illness and can coordinate comprehensive treatment plans rather than focusing solely on antibiotic protocols
Long-term success depends on consistent monitoring and lifestyle foundations, including detailed symptom tracking, regular retesting, quality sleep, stress management, and anti-inflammatory nutrition to support your body’s healing capacity
When your Lyme treatment hits a wall, it’s not because you’re “crazy” or imagining things—there are real, complex reasons behind treatment failures that many doctors simply don’t address.
You’re chasing the “perfect” protocol that doesn’t exist. Here’s the hard truth: there’s no magic bullet for Lyme disease. You might spend months researching the latest antibiotic combinations, hunting down specialized doctors, or trying expensive IV treatments—only to find your symptoms stubbornly persist.
The problem? You’re focusing solely on killing Lyme bacteria while ignoring the bigger picture.
Your Lyme diagnosis became a diagnostic dead end. Once you get that Lyme diagnosis, many doctors stop looking for other culprits. It’s like finding one leaky pipe in your house and declaring the plumbing fixed—meanwhile, mold is growing behind your walls, and your electrical system is shorting out.
You’re throwing money at Lyme-specific treatments. Patients often spend thousands hopping from clinic to clinic, trying every new Lyme protocol they read about online. But what if your fatigue isn’t from Lyme at all? What if it’s actually from toxic mold exposure or a co-infection that requires completely different treatment?
This tunnel vision keeps you trapped in an expensive cycle of ineffective treatments.
Multiple conditions are masquerading as Lyme symptoms. Your body doesn’t operate in neat diagnostic categories. It often travels with toxic mold exposure, heavy metal toxicity, and other stealth infections that create overlapping symptoms.
Think of it like trying to fix a car that’s making strange noises. You might replace the muffler (treat Lyme disease), but if the engine is also knocking (due to co-infections) and the transmission is slipping (resulting from mold toxicity), you’ll still have problems.
Co-infections require their treatment strategies. When that tick bit you, it didn’t just deliver Lyme bacteria—it potentially injected a cocktail of pathogens. Babesia causes symptoms such as air hunger and night sweats. Bartonella triggers neurological symptoms and rage episodes. Rocky Mountain spotted fever creates joint pain that mimics Lyme arthritis.
Standard Lyme antibiotics, such as doxycycline, barely address some of these co-infections. It’s like trying to kill ants with mosquito spray—using the wrong tool for the job.
Your cellular machinery is still broken. Even after successful Lyme treatment, your mitochondria (the cells’ powerhouses) may remain damaged. This cellular dysfunction perpetuates the crushing fatigue, brain fog, and exercise intolerance that define chronic Lyme symptoms.
Studies show that up to 20% of Lyme patients develop post-treatment symptoms, with nearly 100,000 Americans each year left with persistent issues even though following standard protocols. Your immune system might have won the battle against Lyme bacteria, but the war isn’t over until you repair the collateral damage.
Your unique genetics and toxic load matter. Some people cleanse efficiently and bounce back quickly. Others—those with genetic variations affecting methylation or glutathione production—struggle to clear toxins and inflammatory debris. Add chronic stress, poor sleep, or ongoing mold exposure, and your body can’t heal even with “perfect” treatment.
When standard Lyme protocols keep falling short, it’s time to dig deeper into the overlooked culprits that might be sabotaging your recovery.
Mold exposure mimics Lyme symptoms so closely that even experienced doctors get fooled. You’ll experience the same crushing fatigue, joint pain that moves around your body, and that maddening brain fog that makes you forget words mid-sentence.
Here’s what makes this tricky: your immune system is already compromised from fighting Lyme, so it can’t properly cleanse mold toxins. It’s like trying to bail water from a sinking boat while someone keeps pouring more in.
The overlap is staggering. Both conditions trigger similar inflammatory responses, leaving you wondering if your Lyme treatment isn’t working or if something else entirely is making you sick.
Start with your environment. Get an ERMI test for your home—it’ll reveal hidden mold that standard inspections miss. You can also run a urine mycotoxin test to see what’s circulating in your system.
And here’s something most doctors won’t tell you: even after leaving a moldy environment, those toxins can persist for months or years without proper ventilation support.
Some infections can go completely undetected, even when they’re wreaking havoc on your system. These aren’t your typical co-infections that Lyme-literate doctors usually test for.
Clostridium difficile (C. diff) typically causes severe diarrhea in hospitalized patients. But here’s the kicker—it can also exist without any gut symptoms at all, just pumping out toxins that fuel systemic inflammation. You may have C. diff and not even know it.
MARCoNS (Multiple Antibiotic-Resistant Coagulase-Negative Staphylococci) sounds like a mouthful, but it’s essentially a stubborn staph infection that establishes itself in your nasal passages. Some practitioners swear by treating it, while others remain skeptical. But for certain patients, addressing MARCoNS has been transformative.
Push for specific testing. Ask your doctor to run C. diff toxin tests—not just culture tests that might miss toxin-producing strains. For MARCoNS, you’ll need a nasal swab sent to a lab that looks explicitly for this organism.
Don’t let anyone brush off these requests. If you’re still experiencing symptoms after undergoing thorough Lyme treatment, these hidden factors may warrant further investigation.
Your cellular powerhouses take a severe beating from both Lyme bacteria and mold toxins. Think of mitochondria as tiny engines in every cell—when they’re damaged, your whole system runs on empty, no matter how much you rest.
This explains why some people feel exhausted even years after successful Lyme treatment. The infection might be gone, but the cellular damage lingers.
Unconventional therapies are showing promise. Methylene blue treatment (under professional guidance) can help repair mitochondrial function. Supplements like CoQ10, NAD+, and PQQ support cellular energy production from different angles.
Organic acid testing reveals what is truly happening at the cellular level. It shows whether your mitochondria are producing energy efficiently or struggling with specific metabolic pathways.
Work with a functional medicine practitioner who understands mitochondrial medicine—this isn’t something you want to tackle alone.
Sometimes the answer lies in entirely unexpected places. These conditions can masquerade as treatment-resistant Lyme, leaving you chasing the wrong target for months or years.
Condition | Symptoms | Testing Method |
|---|---|---|
Heavy Metal Toxicity | Fatigue, brain fog, neurological issues | Hair analysis, urine provocation test |
Parasitic Infections | Digestive issues, fatigue | Comprehensive stool analysis |
Viral Reactivation | Chronic fatigue, muscle pain | EBV, CMV, or HHV-6 antibody tests |
Heavy metals like mercury from old dental fillings or lead from old paint can cause neurological symptoms that perfectly mimic chronic Lyme. The irony? Some of these metals make infections harder to clear.
Parasites aren’t just a problem in the third world. You can pick them up from contaminated water, undercooked food, or even your beloved pets. They’re masters of hiding and can cause fatigue that rivals any chronic infection.
Viral reactivation happens when your immune system is too busy fighting other battles. Epstein-Barr virus, cytomegalovirus, and human herpesvirus-6 can all reactivate from dormancy and contribute to your symptoms.
The key is comprehensive testing that looks beyond the obvious suspects. Your body might be fighting multiple battles simultaneously, and until you address them all, you’ll stay stuck in the treatment-resistant zone.
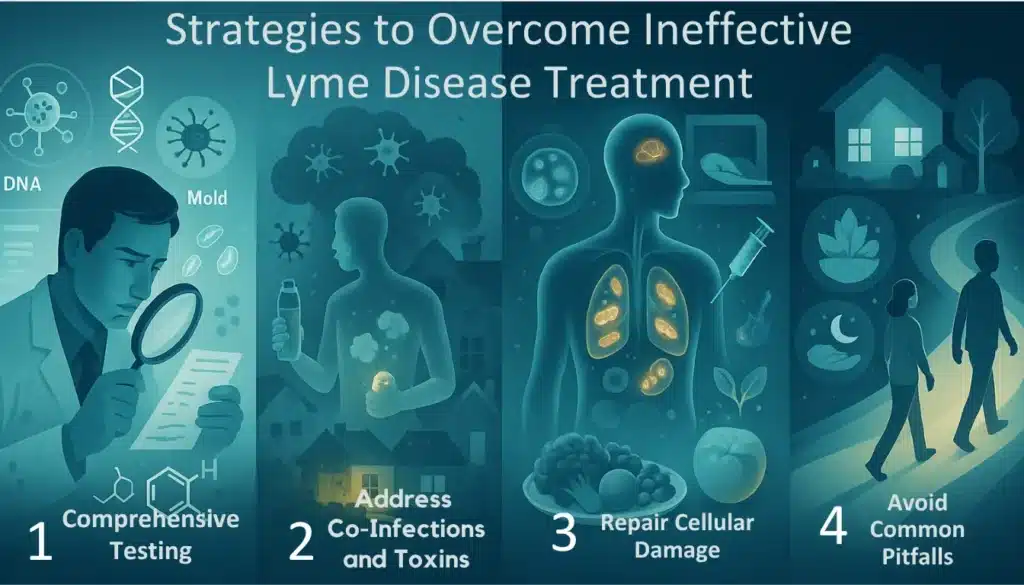
Breaking the cycle of ineffective Lyme disease treatment requires a holistic approach that goes beyond standard protocols. Success comes from uncovering all root causes and systematically addressing them rather than chasing symptoms.
Think of testing like detective work—you’re gathering clues to solve a complex mystery. Standard Lyme tests often miss the bigger picture, leaving you with incomplete information.
Online tools, such as symptom quizzes, can help identify potential root causes based on your specific symptoms and suggest relevant laboratory tests. These aren’t diagnostic tools, but they’re incredibly helpful for mapping out your testing strategy.
Co-infection panels test for Babesia, Bartonella, and other tick-borne pathogens that standard Lyme antibiotics may not address. These sneaky bugs often fly under the radar while keeping you sick.
Mycotoxin urine tests can reveal mold exposure that may be mimicking or exacerbating your Lyme symptoms. You’d be surprised how many “treatment-resistant” cases involve mold toxicity.
C. diff toxin tests and MARCoNS nasal swabs uncover hidden infections that can sabotage your recovery. These bacterial troublemakers love to hide in your gut and sinuses.
Mitochondrial function tests (like organic acid tests) show whether your cellular powerhouses are working correctly. When your mitochondria are damaged, you’ll feel exhausted no matter what treatment you try.
The key here? Work with a Lyme-literate or functional medicine practitioner who thinks beyond the standard Lyme box. They’ll order the proper tests and know how to interpret the results.
Treating Lyme while ignoring co-infections is like trying to fix a leaky roof while ignoring the broken pipes. You’ll never get ahead.
Treating all identified co-infections simultaneously is vital because untreated pathogens create a constant state of immune chaos. Each infection feeds off the others, creating a vicious cycle that keeps you trapped in chronic illness.
Detoxification becomes your best friend. Support your body’s natural refresh pathways with binders like activated charcoal or specialized mold binders. Think of these as tiny sponges that soak up toxins before they can cause further damage.
Hydration matters more than you’d think—aim for half your body weight in ounces of clean water daily. Your kidneys require adequate hydration to effectively flush out toxins.
Sauna therapy (if tolerated) helps your body sweat out toxins through the skin. Start slowly—some people may feel worse initially as toxins are mobilized.
Environmental changes can significantly impact your recovery. If testing reveals mold in your living space, you’ll need to either remediate thoroughly or relocate to a mold-free environment. Staying in a moldy home while trying to treat mold illness is like trying to fill a bucket with holes in it.
Your cells are like tiny factories—when they’re damaged, everything else falls apart. Mitochondrial repair isn’t just helpful; it’s essential for lasting recovery.
Incorporate targeted nutrients, such as CoQ10, L-carnitine, and alpha-lipoic acid, to restore energy production at the cellular level. These aren’t just supplements—they’re the raw materials your mitochondria need to function correctly.
Your diet becomes medicine. Adopt an anti-inflammatory approach rich in whole foods and low in processed sugars. Every meal either feeds inflammation or fights it—there’s no neutral ground.
Emerging therapies, such as methylene blue, show promise for mitochondrial repair, but should only be explored under proper medical supervision. These treatments can be powerful but require careful monitoring.
Sleep quality trumps sleep quantity. Eight hours of poor sleep won’t help your cells repair themselves. Focus on maintaining good sleep hygiene, regulating room temperature, and minimizing blue light exposure before bedtime.
Doctor-hopping is expensive and exhausting. Constantly switching practitioners in search of the “perfect” Lyme protocol wastes precious time and money while keeping you stuck in treatment limbo.
Many patients fall into the trap of ignoring lifestyle factors while pursuing complex treatments. Poor sleep, chronic stress, or inflammatory diet choices can completely undermine even the best treatment protocols.
The solution? Partner with one thorough practitioner who takes a comprehensive approach. Give them time to work through your case systematically rather than jumping ship at the first sign of slow progress.
Prioritize the basics alongside your treatment plan. Consistent sleep, stress management, and proper nutrition aren’t just “nice to have“—they’re essential foundations that determine whether your treatments will work.
Remember: Recovery isn’t linear, and there’s no one-size-fits-all approach. What matters is finding someone who’ll dig deep enough to uncover your unique combination of root causes and address them systematically.
Recovery from Lyme disease treatment failure requires patience and a multi-faceted approach. Think of it like rebuilding a house after a storm—you need the right team, the right tools, and a solid blueprint.
Finding the right practitioners can make or break your recovery journey. You wouldn’t trust a general contractor to rewire your entire electrical system, so why settle for doctors who don’t truly understand complex chronic illness?
Lyme-literate doctors should be your priority. These practitioners have spent years studying the intricate dance between Borrelia bacteria, co-infections, and immune dysfunction. They understand that 10-30% of patients experience persistent symptoms after standard treatment, and they’re equipped to dig deeper.
Look for functional medicine training on their credentials. These doctors view the body as an interconnected system rather than a collection of isolated symptoms. They’ll investigate why your immune system isn’t clearing infections and what’s preventing your mitochondria from producing energy.
Specialized consultants become essential when you’re dealing with multiple root causes. Mold experts can identify environmental toxins that mimic the symptoms of Lyme disease. Infectious disease specialists familiar with biofilms and persister cells offer advanced treatment protocols. Mitochondrial health practitioners focus on cellular repair—the foundation of lasting recovery.
Here’s what I’ve learned: don’t put all your eggs in one basket. Your primary Lyme-literate doctor should coordinate care, but specialized consultants fill critical gaps.
Tracking your recovery isn’t just helpful—it’s essential for identifying what works for you. Without data, you’re flying blind through treatment protocols that cost thousands of dollars.
Keep a detailed symptom journal that goes beyond “I felt bad today.“ Rate your energy levels, brain fog, joint pain, and sleep quality on a 1-10 scale. Note what treatments you’re taking, dietary changes, stress levels, and even weather patterns.
I’ve seen patients discover that their worst flare-ups coincide with mold exposure from seasonal rains or that certain supplements worsen their symptoms. These patterns become invisible without consistent tracking.
Laboratory retesting every 3-6 months provides objective data about your progress. Co-infection levels, inflammatory markers, and mycotoxin levels are expected to improve over time. If they’re not, something in your protocol needs adjusting.
Don’t get discouraged if progress feels slow. Recovery from chronic Lyme isn’t linear—you might feel worse before you feel better as your body eliminates toxins and dead bacterial debris.
Healing from chronic Lyme disease is an ongoing process, not a fixed destination. Conventional treatments often fall short, but it’s possible to dig deeper and uncover hidden causes like mold, co-infections, or cellular issues.
Persistent symptoms are clues guiding you to the root issues. Keep a symptom journal to track patterns that offer valuable insights. Healing isn’t straightforward, but with patience and the right tools, you can address your body’s complexities. Celebrate progress, trust your intuition, and stay committed to finding what truly helps you heal. Partner with practitioners who understand it.
Find doctors who understand that chronic illness rarely has a single cause or a one-size-fits-all solution. They should be willing to dig deeper when Plan A doesn’t work, not just shrug and suggest it’s all in your head.
The path forward may not always be clear, but it exists. And you’ve got everything you need to find it.
Treatment failure can occur due to various overlooked factors, including co-infections, mold exposure, immune dysfunction, and cellular damage. Many doctors focus solely on killing Lyme bacteria while missing other underlying conditions that mimic or complicate Lyme symptoms. Individual genetics and toxic load also play crucial roles in treatment response.
The main reasons include undiagnosed co-infections that require specific treatments, toxic mold exposure mimicking Lyme symptoms, mitochondrial dysfunction causing persistent fatigue, and doctors stopping their search for other causes once Lyme is diagnosed. Standard antibiotics may not address these complex underlying issues.
Mold toxicity can mimic Lyme symptoms and create additional immune system stress, making recovery more difficult. Patients may continue experiencing fatigue, brain fog, and other symptoms even after Lyme treatment if mold exposure isn’t addressed. Environmental mold testing and mycotoxin urine tests can help identify this hidden factor.
Common co-infections include Babesia, Bartonella, Ehrlichia, and Anaplasma, which require specific antimicrobial protocols. Hidden infections, such as C. diff and MARCoNS (antibiotic-resistant staph in the nasal passages), can also complicate recovery. Comprehensive co-infection testing is essential for developing an effective treatment plan.
Mitochondria are cellular powerhouses that produce energy. When damaged by infections or toxins, they can’t function properly, leading to persistent fatigue, brain fog, and other symptoms. Even after successful Lyme treatment, mitochondrial repair may be necessary for full recovery through targeted nutrients and cellular support.
Key tests include comprehensive co-infection panels, mycotoxin urine tests, mitochondrial function assessments, and environmental mold testing. Additional tests may consist of heavy metal panels, genetic testing for detoxification pathways, and comprehensive stool analysis to identify gut infections or dysbiosis.
Recovery is highly individual and depends on factors like duration of illness, co-infections, toxic load, and personal genetics. Some patients see improvement within months, while others may require years of comprehensive treatment. Recovery is rarely linear and requires patience, persistence, and a multi-faceted approach.
Keep detailed symptom journals, noting daily symptoms, energy levels, and responses to treatment. Regular laboratory retesting can monitor infection markers and immune function. Work with your practitioner to establish baseline measurements and track improvements over time through objective markers and symptom patterns.
Alexander W. 2012 integrative healthcare symposium: treating the pain of lyme disease and adopting lifestyle change as therapy. P T. 2012 Apr;37(4):247-9. PMID: 22593637; PMCID: PMC3351864.
Prato, D., Smith, A., & Oertle, J. (2014). Chronic Lyme Disease: Persistent Clinical Symptoms Related to Immune Evasion, Antibiotic Resistance and Various Defense Mechanisms of Borrelia burgdorferi. Open Journal of Medical Microbiology, 04, 252-260. https://doi.org/10.4236/OJMM.2014.44029.
Cincotta, A., & McManus, M. (2015). Effects of Borrelia on host immune system: Possible consequences for diagnostics. Advances in integrative medicine, 2, 81-89. https://doi.org/10.1016/J.AIMED.2014.11.002.
We have helped thousands of
people restore their health
and quality of life by diagnosing
and treating their Lyme Disease.
“Dr. Mueller’s approach to medicine is refreshing! There is only so much you can do with western medicine and in my life I was needing a new approach. By addressing the whole body, nutritional diet factors, environmental factors, blood work, and incorporating ideas I had not previously known, I was able to break through with my conditions. I am not only experiencing less pain in my life, but through the process of healing guided by Dr. Diane Mueller, I am now happy to say I have more consciousness surrounding how I eat, what to eat and when things are appropriate. Living by example Dr. Mueller has a vibrancy that makes you want to learn and know more about your body and overall health. I highly recommend her to anyone looking for new answers, a new approach to health, or in need of freedom from pain and limitations.”
-Storie S.
Kihei, HI
